Bloodborne pathogens (BBPs) are microscopic organisms – viruses, bacteria, and parasites – present in human blood and certain bodily fluids. These pathogens can cause serious and potentially life-threatening infections if they enter the bloodstream of a susceptible person. Healthcare professionals, first responders, and anyone who may come into contact with blood or other potentially infectious materials (OPIM) at work are at increased risk of exposure.
This blog serves as an educational resource for understanding the risks associated with BBPs, the importance of universal precautions, and proper disposal procedures for contaminated materials. By implementing these protocols, we can create safer work environments for ourselves and our colleagues.
Understanding Bloodborne Pathogens
In healthcare settings, several bloodborne pathogens pose significant risks to both patients and healthcare workers. Among the most prevalent are:
- Hepatitis B (HBV): HBV infectioncan result in acute or chronic liver disease, potentially leading to severe complications such as liver damage, cirrhosis, and hepatocellular carcinoma.
- Hepatitis C (HCV): Chronic HCV infectioncan cause progressive liver damage, including fibrosis and cirrhosis, and may eventually lead to liver failure or hepatocellular carcinoma.
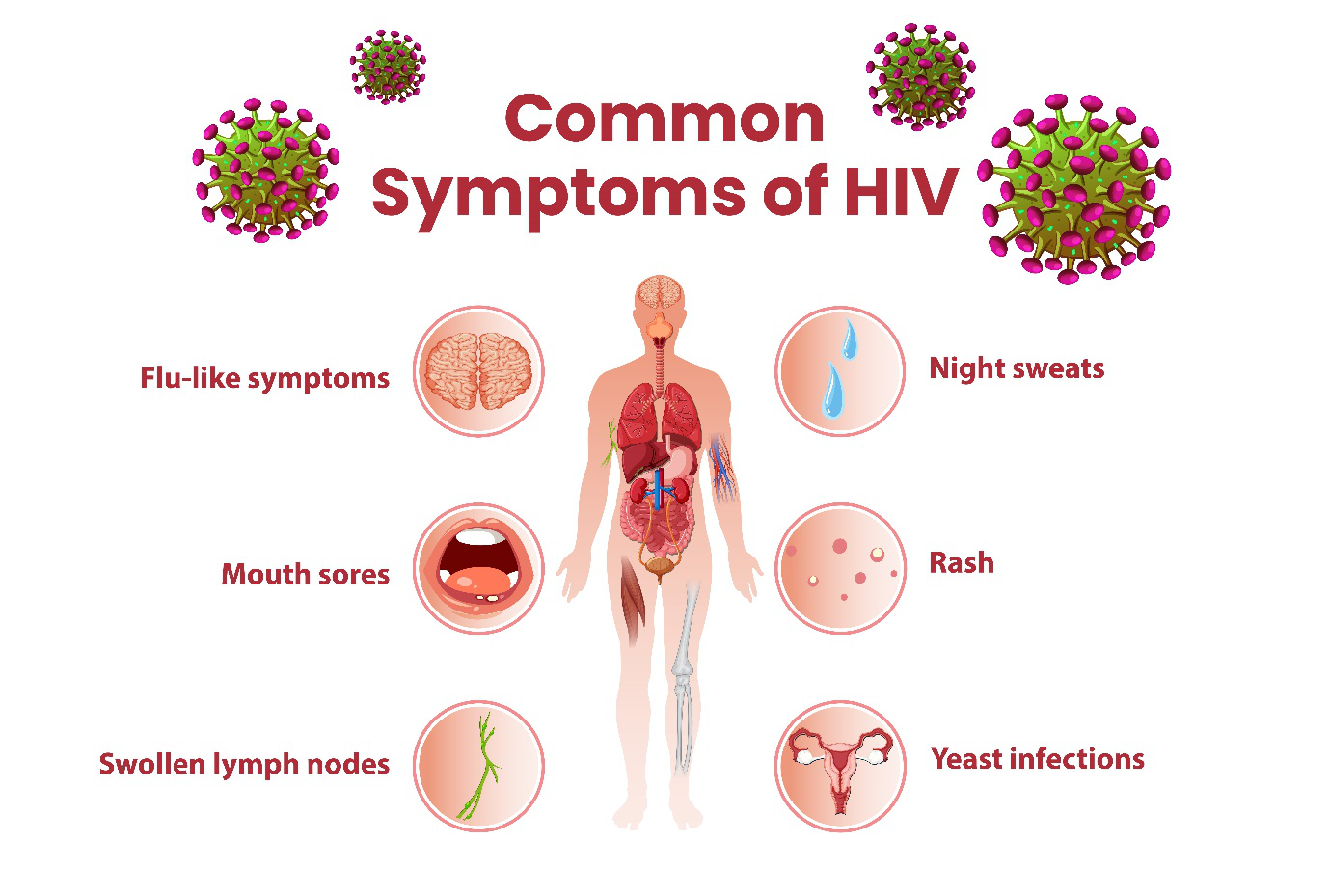
- Human Immunodeficiency Virus (HIV):HIV targets the body’s immune system, ultimately leading to Acquired Immunodeficiency Syndrome (AIDS), a condition characterized by increased susceptibility to infections and certain cancers.
Transmission of these pathogens can occur through various routes, including:
- Percutaneous Exposure:This route involves the entry of bloodborne pathogens directly into the bloodstream through puncture wounds, such as needlestick injuries, cuts, or abrasions. Healthcare workers are particularly vulnerable to percutaneous exposures during procedures involving needles or sharp instruments.
- Mucous Membrane Exposure:Blood or other potentially infectious materials (OPIM) splashed or sprayed into the eyes, nose, or mouth can result in the transmission of bloodborne pathogens. While less common than percutaneous exposure, mucous membrane exposure still poses a significant risk, particularly during procedures with a high potential for splashes or aerosolization.
- Sexual Contact:While less relevant in most workplace settings, healthcare workers may face an increased risk of HIV transmission through sexual contact if they come into contact with contaminated bodily fluids.
It’s essential to recognize that the presence of visible blood is not always necessary for transmission to occur. Bodily fluids such as cerebrospinal fluid, synovial fluid, pleural fluid, and pericardial fluid can also contain significant concentrations of bloodborne pathogens, highlighting the importance of exercising caution and implementing appropriate infection control measures at all times.
Universal Precautions: Protecting Against Bloodborne Pathogens
Universal precautions are a cornerstone of infection control practices in healthcare settings and other high-risk industries where exposure to bloodborne pathogens is a concern. These precautions are designed to protect healthcare workers, first responders, and other employees from potential exposure to infectious materials and to prevent the transmission of bloodborne diseases. By adhering to universal precautions, individuals can minimize the risk of infection and ensure the safety of themselves and their colleagues.
- Hand Hygiene:Proper hand hygiene is fundamental to preventing the spread of bloodborne pathogens and other infectious diseases. Healthcare professionals and first responders should wash their hands thoroughly with soap and water for at least 20 seconds before and after patient contact, after removing gloves, and after any potential exposure to blood or bodily fluids. Alcohol-based hand sanitizers can also be used as an alternative when handwashing facilities are not readily available.
- Personal Protective Equipment (PPE):Personal protective equipment (PPE) plays a crucial role in protecting against exposure to bloodborne pathogens. Healthcare workers and first responders should wear appropriate PPE, including gloves, gowns, masks, and eye protection, when handling blood or bodily fluids or when performing procedures with a risk of exposure. Gloves should be changed between patient contacts and replaced immediately if torn or punctured to prevent contamination.
- Safe Injection Practices:Safe injection practices are essential for preventing needle stick injuries and the transmission of bloodborne pathogens. Healthcare workers should use single-use, disposable needles and syringes for each patient encounter and avoid recapping needles by hand. Sharps should be disposed of in puncture-resistant containers immediately after use to minimize the risk of needle stick injuries.
- Safe Handling of Contaminated Materials:Proper handling and disposal of contaminated materials are critical components of infection control. Contaminated materials, such as used needles, blood-soaked dressings, and other medical waste, should be disposed of promptly in leak-proof, labeled containers. Employers should provide clear guidance on the proper segregation and disposal of different types of waste to prevent accidental exposure to bloodborne pathogens.
- Environmental Controls:Employers should implement environmental controls to minimize the risk of exposure to bloodborne pathogens in the workplace. This may include proper cleaning and disinfection of surfaces and equipment, particularly in areas where procedures involving blood or bodily fluids are performed. Spills of blood or bodily fluids should be cleaned up promptly using appropriate disinfectants to reduce the risk of contamination.
Proper Disposal Procedures
Proper disposal of contaminated materials is crucial for preventing the spread of bloodborne pathogens and protecting workers and the public from exposure to infectious materials. Employers must ensure that employees are adequately trained in the correct disposal procedures and have access to the necessary equipment and supplies for safe disposal.
1. Use of Sharps Containers:
Used needles, syringes, lancets, and other sharp objects pose a significant risk of needlestick injuries and potential transmission of bloodborne pathogens. Therefore, it is imperative to immediately place these items into puncture-resistant sharps containers after use. Sharps containers should be readily available in areas where procedures involving sharps are performed, such as patient rooms, medical clinics, and laboratories. Additionally, sharps containers should be securely closed when full to prevent spills or accidental exposure.
2. Segregation of Waste:
Contaminated materials, including blood-soaked dressings, bandages, gloves, and other medical waste, must be segregated from regular waste to prevent cross-contamination and exposure to infectious materials. It is essential to use leak-proof, labeled containers designated specifically for the disposal of biohazardous waste. These containers should be clearly marked with biohazard symbols to alert individuals to the potential presence of hazardous materials.
3. Disposal of Regulated Medical Waste:
Regulated medical waste, which includes blood-contaminated materials, sharps, and microbiological waste, must be disposed of in accordance with local regulations and guidelines. Employers are responsible for arranging the safe collection, transportation, and disposal of regulated medical waste through licensed waste management providers. These providers ensure that medical waste is treated and disposed of properly to prevent environmental contamination and protect public health.
4. Chemical Disinfection of Contaminated Surfaces:
In addition to proper disposal of contaminated materials, it is essential to disinfect surfaces that may have come into contact with blood or bodily fluids to prevent the spread of pathogens. Employers should provide appropriate disinfectants effective against bloodborne pathogens, such as bleach solutions or EPA-approved disinfectants, for cleaning and decontamination purposes. Surfaces should be thoroughly cleaned and disinfected according to manufacturer instructions and regulatory guidelines to ensure the elimination of infectious agents.

A graphic illustrating the steps to take for safe disposal of PPE and other items after being exposed to BBPs.
5. Incineration or Autoclaving of Infectious Waste:
Some types of regulated medical waste, such as certain sharps and microbiological materials, may require specialized treatment methods, such as incineration or autoclaving, to render them safe for disposal. Employers should arrange for the proper treatment and disposal of infectious waste through licensed medical waste disposal facilities equipped with the necessary equipment and expertise to handle bio hazardous materials safely.
Incineration and autoclaving processes effectively destroy pathogens and reduce the volume of waste, minimizing the risk of environmental contamination and exposure to infectious agents.
6. Training and Education:
All employees who handle contaminated materials must receive comprehensive training on proper disposal procedures and infection control practices. Training should cover the use of personal protective equipment (PPE), safe handling techniques, and protocols for cleaning and disinfecting work areas. Employees should also be educated on the importance of adhering to disposal guidelines to prevent exposure to bloodborne pathogens and minimize the risk of workplace accidents and injuries.
7. Monitoring and Compliance:
Employers should establish monitoring systems to ensure compliance with proper disposal procedures and infection control practices. Regular inspections of waste disposal areas, including sharps containers and biohazardous waste storage areas, can help identify potential hazards or compliance issues. Additionally, employers should provide ongoing education and reinforcement of disposal protocols to maintain a culture of safety and accountability in the workplace.
Enrol Now in Metro Safety’s First Aid Training Courses!
Metro Safety is committed to equipping workers with the theoretical knowledge and practical skills necessary to protect themselves against bloodborne pathogens in the workplace. Through our comprehensive training programs, participants learn about the risks associated with bloodborne pathogens, universal precautions, and proper disposal procedures for contaminated materials.
To this end, we offer a number of first aid training programs, including our occupational first aid courses (Levels 1 through 3), emergency and standard first aid courses, both of which are vetted by the Canadian Red Cross, and a number of workplace safety courses; fall protection and inspection, confined space safety, and forklift operation among others.
Visit our website today and explore our courses to find the one that fits your requirements.